ImpairmentCheck® helps claims professionals and attorneys improve the accuracy of impairment ratings based on the AMA Guides to the Evaluation of Permanent Impairment. It is a screening and educational tool that provides guidance on probable impairment for most ratable injuries while also collecting data for continuous quality improvement.
The system is based on our own patented, web-based technologies (8,185,410; 8,615,411). Think of it as a part subject-matter expert (SME), part artificial intelligence (AI), and part machine learning. Or don’t think of any of that; just let it help improve the efficiency and quality of your work, along with the reliability and accuracy of your reports. We’ve made it easy!
Why Impairment Check?
Inflated impairment ratings and resulting permanent partial disability awards result in substantial financial costs for payers and human costs by creating a perception that someone is significantly damaged. Approximately 40% of indemnity payments.[i] Unfortunately, many impairment ratings are inaccurate. More often, they are higher than appropriate, resulting in unnecessary costs and sometimes diverting resources from those who would be best served. Occasionally, they are too low, resulting in lower benefits than is fair.
These inaccuracies may result from bias, flawed clinical and/or causation analysis, and misapplication of the AMA Guides to the Evaluation of Permanent Impairment. Robber Bonner, MD, who was Vice President for Hartford, estimated that carriers could save as much as 10% on permanent partial disability payouts by assuring accurate ratings.[ii]
Erroneous Ratings – How Serious Is This Issue?
Errors can be identified by having impairment assessments and associated clinical data evaluated by impartial experts skilled in the use of the AMA Guides. Impairment ratings are expressed as whole person or as regional impairments. Whole person impairment (WPI) ratings range from 0 (normal) to 100% (death). The values per rating unit vary based on jurisdiction and average weekly wage; however, they are typically in the range of $1,400 to $2,100 per point (average $1,750 per WPI unit).
Error rates are higher in jurisdictions where evaluators are unskilled and/or biased, litigation is high, and/or an older Edition of the AMA Guides is used, e.g., California. Typically, errors result in inflated ratings. Melissa Starnes reported in 2015 that a study of a client found a 17% error rate and a difference between the correct rating and the erroneous rating of 16% WPI. Bonner reported an overall 15% error rate and a 7% WPI difference. Overall, based on these three studies and other anecdotal reports, it is probable that at least 20% of ratings are incorrect, with those cases reflecting an overrating of approximately 10% WPI.
What Are Potential Savings?
Assuming an average value of $1,750 per rating unit, if these errors were identified and effectively managed, there would be savings of $17,500 per erroneous case. Therefore, per 100 cases, the potential savings would be approximately $350,000 (20 x $17,500). For an insurer or third-party administrator with 10,000 impairment rating cases, the potential is $35 million; assuming a success rate of 50%, the potential savings is $17.5 million.
What are Best Practices, and Why is Impairment Check the Critical Component?
Best practices involve carefully designed, cost-efficient processes to assure accurate ratings. This includes: 1) assuring accurate impairment ratings (i.e., preventing erroneous ratings), 2) detecting erroneous ratings, and 3) managing erroneous ratings. Principles of total quality improvement must be applied. All stakeholders (e.g., claims staff, medical teams, physicians, and attorneys) should understand the basics of impairment rating and ensure accurate ratings.
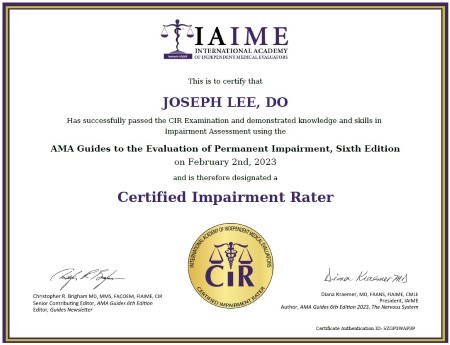
Accurate impairment ratings are more likely if they are performed by skilled, unbiased evaluators who are trained in the use of the AMA Guides, are certified to perform impairment ratings, and are provided with guidance and standards.
All impairment ratings should be screened initially using technology and triaged. If it is probable a rating is accurate, no further action is required. If it is likely that it is erroneous, the case should be analyzed by an experienced evaluator, and appropriate medical and legal strategies applied.
ImpairmentCheck® allows users to enter an impairment rating value for a diagnosis, which then engages the program in generating a graph showing whether or not the rating is reasonable. In addition, immediate guidance is provided regarding the management of the rating, clinical issues pertinent to impairment, maximum medical improvement (MMI), the specifics of the impairment assessment process, as well as information on the most common errors and how to manage them.
It can be efficiently integrated into a best practice impairment assessment management process. It can also be used to project the magnitude of impairment associated with a diagnosis; such information is very useful in reserving cases. The likelihood of obtaining an accurate impairment rating is enhanced by printing information for a diagnosis and providing this to the evaluating physician.
Lastly, educational video content is provided on the rating process, and users have access to monthly Question and Answer sessions with Christopher R. Brigham, MD, Editor of the Guides Newsletter and AMA Guides, Sixth Edition, and the primary developer of this software system.
ImpairmentCheck® is not the same as software systems designed for physicians to be used in developing a rating, e.g., Cedaron, EME International, JTech, etc. The purpose and design of this are entirely different; it is similar to comparing “apples and oranges” since the two cannot be practically compared. Impairment Check is designed for claims professionals, and software rating systems are designed for physicians. Impairment rating systems designed for physicians require incorporating valid and reliable data to develop a rating. Unfortunately, the data entered may be inaccurate, and thus, the rating is inaccurate; i.e., “GIGO – Garbage In, Garbage Out.” Impairment Check, designed for claims professionals, provides data and information on the injuries and illnesses most commonly seen. As opposed to physician rating software systems, it provides information on the typical rating value seen, information on pertinent clinical issues, reference to criteria in the Guides, a narrative explanation of the rating process, and a discussion of the most common errors. In addition, it provides information that can be shared with physicians and other stakeholders, as well as learning experiences.
ImpairmentCheck® is an essential tool for ensuring accurate ratings.
“We are convinced that all stakeholders will experience more accurate impairment ratings by using Impairment Check, which is empowered by the congruence of data, information, and patented technologies. Impairment Check revolutionizes how we manage impairment ratings and creates a new industry-standard paradigm,” – Christopher R. Brigham, MD, President of Brigham and Associates, Inc., and Senior Contributing Editor of the “AMA Guides to the Evaluation of Permanent Impairment” Sixth Edition, and Editor of the “Guides Newsletter”
Want to View a Demo?
View 2 1/2 minute Impairment Check demo video.
Want to Learn More?
Contact us at support@cbrigham.com to learn more.
References
[i] Starnes M. Are Your Impairment Ratings Impaired (Less Than Perfect. WorkCompWire. September 1, 2015 https://www.workcompwire.com/2015/09/melissa-starnes-are-your-impairment-ratings-impaired-less-than-perfect/
[ii] Kamin JP. Faulty Impairment Ratings Creating Substantial Costs for Carriers. WorkCompCentral. August 21, 2012.
[iii] Brigham Cr, Uejo C, Dilbeck L, Uehlein WF. Impairment Ratings: Observations Based on Review of More Than 6,000 cases. Guides Newsletter. March / April 2010.